Experiencing sharp shooting pain in the private area can be distressing for females, often indicating underlying issues that require attention. This type of pain is typically characterized by sudden, intense sensations in the pelvic region, including the vagina, vulva, or nearby areas.
Healthcare experts stress the importance of promptly seeking medical advice when encountering such symptoms. They recommend a thorough evaluation by a healthcare provider to determine the precise cause of the pain, as it can stem from various conditions ranging from benign to more serious health concerns.
Early diagnosis and proper management are crucial to addressing the root cause and ensuring appropriate treatment.
What is Pelvic Pain?
Pelvic pain refers to discomfort or sharp, stabbing sensations in the lower abdominal area, specifically around the pelvic region. It can manifest in various forms and intensities, often indicating underlying issues that range from menstrual cramps to more serious gynecological or reproductive conditions.
Understanding the specific characteristics of pelvic pain can help in identifying potential causes and seeking appropriate medical advice promptly.
Sharp, stabbing pain in the uterus (not pregnant): This type of pain can occur due to conditions such as menstrual cramps, uterine fibroids, or pelvic inflammatory disease (PID).
Sudden stabbing pain in the pelvic area on the female left side: Pain on the left side of the pelvic area could be caused by conditions like ovarian cysts, endometriosis, or even gastrointestinal issues.
Sudden stabbing pain in the pelvic area on the female right side: Pain on the right side may indicate issues such as appendicitis, ovarian cysts, or ectopic pregnancy, among other potential causes.
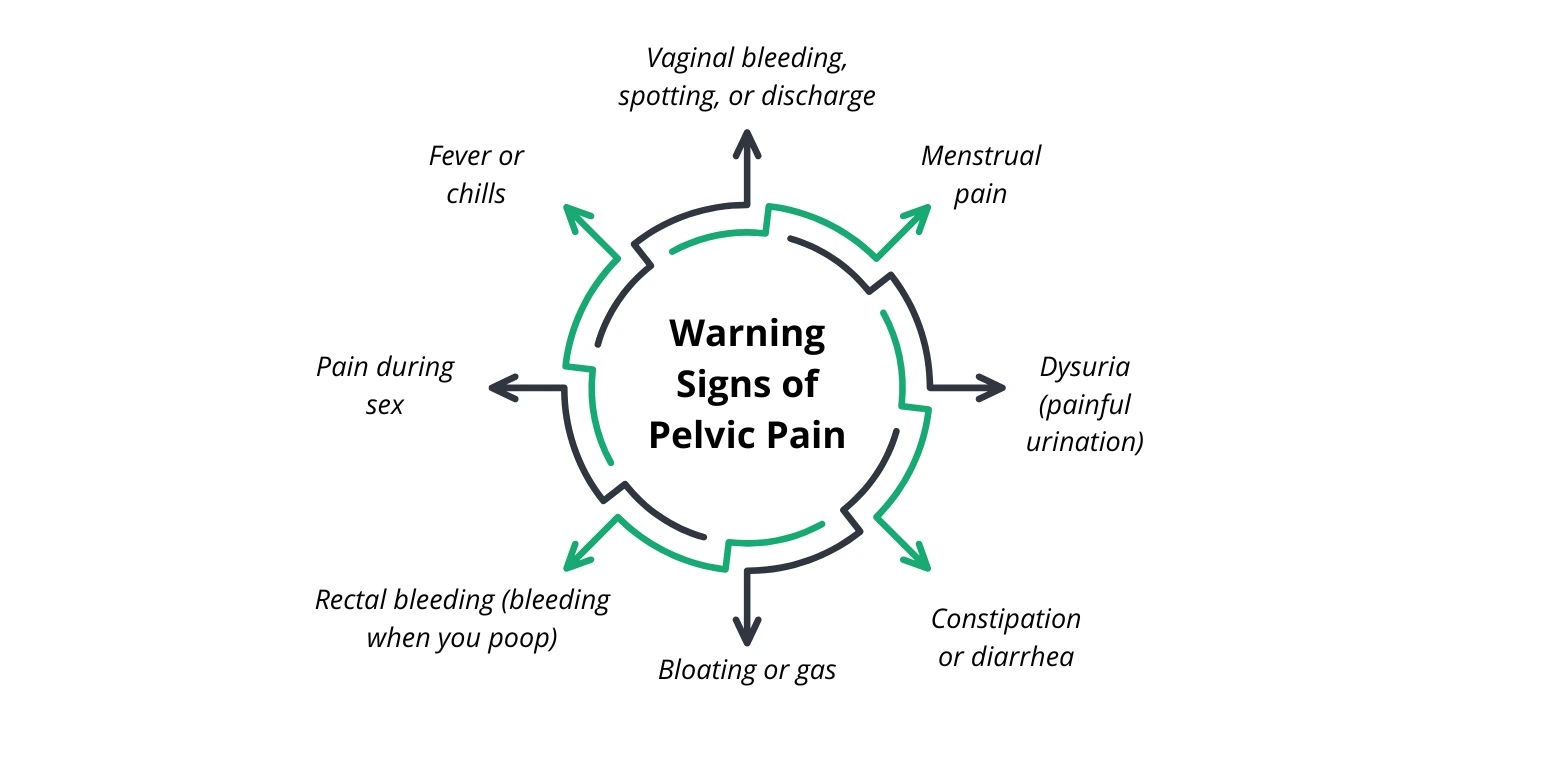
Warning Signs of Pelvic Pain
Recognizing warning signs associated with pelvic pain is crucial for early detection and appropriate management of potential health issues. These signs encompass a range of symptoms that can indicate various underlying conditions affecting the pelvic region.
Being aware of these symptoms can prompt timely medical evaluation, ensuring effective treatment and prevention of complications.
Vaginal bleeding, spotting, or discharge: Abnormal vaginal bleeding, spotting between periods, or unusual discharge can indicate conditions such as infections, hormonal imbalance, or reproductive organ issues.
Menstrual pain: Severe menstrual cramps or pain that significantly affects daily activities may signal conditions like endometriosis or uterine fibroids.
Dysuria (painful urination): Pain or discomfort during urination may be indicative of urinary tract infections (UTIs), pelvic inflammatory disease (PID), or other urinary tract issues.
Constipation or diarrhea: Persistent bowel irregularities can be linked to conditions affecting the digestive system or pelvic organs.
Bloating or gas: Chronic bloating or frequent gas may accompany pelvic pain and could be related to gastrointestinal disorders or reproductive health issues.
Rectal bleeding (bleeding when you poop): Bleeding from the rectum could suggest conditions like hemorrhoids, anal fissures, or inflammatory bowel disease (IBD).
Pain during sex: Painful intercourse, known as dyspareunia, may result from conditions affecting the pelvic organs, such as endometriosis or pelvic inflammatory disease.
Fever or chills: Fever accompanied by pelvic pain could indicate an infection or inflammatory condition that requires medical attention.
10 Common Causes of Sharp Pain in the Vaginal Area
Experiencing sharp pain in the vaginal area can be indicative of various underlying conditions, ranging from benign to more serious health issues. Understanding these potential causes is essential for seeking appropriate medical advice and treatment.
Pelvic Inflammatory Disease (PID)
Pelvic inflammatory disease (PID) is an infection of the female reproductive organs, typically caused by bacteria transmitted through sexual activity or other means. The infection can lead to inflammation and scarring of the fallopian tubes, uterus, and surrounding tissues, causing sharp pelvic pain.
Symptoms may include pain during intercourse or urination, abnormal vaginal discharge, fever, and irregular menstrual bleeding. Prompt medical treatment with antibiotics is crucial to prevent complications such as chronic pelvic pain, infertility, or ectopic pregnancy.
Urinary Tract Infections (UTIs)
Urinary tract infections (UTIs) are common bacterial infections that can affect any part of the urinary system, including the urethra, bladder, ureters, and kidneys. Sharp pain or a burning sensation during urination (dysuria) is a hallmark symptom of UTIs. In some cases, the pain may radiate to the vaginal area due to the proximity of the urinary tract.
Other symptoms may include increased frequency of urination, cloudy or bloody urine, and pelvic discomfort. Treatment typically involves antibiotics prescribed based on the type of bacteria causing the infection.
Ovarian Cysts
Ovarian cysts are fluid-filled sacs that can develop on or within the ovaries. While many cysts are harmless and resolve on their own, others can cause sharp, sudden pain in the pelvic area if they rupture, bleed, or become twisted (ovarian torsion). The pain may be localized to one side of the lower abdomen and can worsen during menstruation or intercourse.
Other symptoms may include pelvic pressure, bloating, and irregular menstrual periods. Monitoring through ultrasound and sometimes surgical intervention is necessary for larger cysts or those causing significant symptoms.
Endometriosis
Endometriosis is a chronic condition where tissue similar to the lining of the uterus (endometrium) grows outside the uterus, commonly on the ovaries, fallopian tubes, or other pelvic organs. This misplaced tissue responds to hormonal changes during the menstrual cycle, leading to inflammation, scarring, and adhesions that can cause severe pelvic pain.
The pain associated with endometriosis is often described as sharp, stabbing, or cramping and may intensify during menstruation, intercourse, or bowel movements.
Other symptoms include excessive menstrual bleeding, infertility, and gastrointestinal issues. Treatment options range from pain medication and hormonal therapy to surgical removal of endometrial implants.
Uterine Fibroids
Uterine fibroids are noncancerous growths that develop within the muscular wall of the uterus. These growths can vary in size and number, causing symptoms such as sharp pelvic pain if they press on nearby organs or nerves. The pain may be intermittent and exacerbated during menstruation or sexual intercourse.
Other symptoms of uterine fibroids include heavy menstrual bleeding, pelvic pressure or fullness, and frequent urination. Treatment options depend on the size, location, and severity of symptoms and may include watchful waiting with monitoring, medication to control symptoms, or surgical removal of the fibroids (myomectomy or hysterectomy).
Vulvodynia
Vulvodynia is a chronic pain condition characterized by a sharp, burning, or stinging pain in the vulva (the external female genitalia). The pain may occur spontaneously or be triggered by touch (such as during intercourse), prolonged sitting, or wearing tight clothing.
The exact cause of vulvodynia is often unknown but may involve nerve sensitivity, muscle spasms, or hormonal changes. Symptoms can vary in intensity and duration, affecting daily activities and sexual function. Treatment may include topical medications, physical therapy, nerve blocks, or counseling to manage pain and improve quality of life.
Interstitial Cystitis (IC)
Interstitial cystitis, also known as painful bladder syndrome, is a chronic condition characterized by pelvic pain, pressure, or discomfort related to the bladder. Sharp pain in the vaginal area can occur alongside symptoms such as urinary urgency, frequency, or pain during urination. IC may be linked to inflammation of the bladder lining or dysfunction of the pelvic floor muscles.
Diagnosis often involves ruling out other conditions with similar symptoms through urine tests, cystoscopy, and bladder biopsies. Treatment options include lifestyle changes, medications to reduce bladder inflammation, physical therapy, and in some cases, procedures to relieve symptoms.
Pelvic Organ Prolapse
Pelvic organ prolapse occurs when the pelvic floor muscles weaken and fail to support the pelvic organs (such as the uterus, bladder, or rectum), causing them to descend or bulge into the vaginal canal. This can lead to sharp pelvic pain, especially during activities that increase intra-abdominal pressure, such as lifting heavy objects or straining during bowel movements.
Other symptoms may include a feeling of heaviness or pressure in the pelvis, urinary incontinence, and difficulty emptying the bladder or bowels. Treatment options range from pelvic floor exercises (Kegel exercises) and pessaries to surgical repair, depending on the severity of prolapse and symptoms.
Ectopic Pregnancy
An ectopic pregnancy occurs when a fertilized egg implants outside the uterus, commonly in the fallopian tubes. Sharp, stabbing pain in the lower abdomen or pelvic area is a hallmark symptom of an ectopic pregnancy, often accompanied by vaginal bleeding, dizziness, or shoulder pain. If left untreated, an ectopic pregnancy can cause life-threatening complications such as internal bleeding.
Diagnosis involves blood tests to measure pregnancy hormones (hCG levels), ultrasound imaging, and sometimes exploratory surgery. Treatment typically involves medication to dissolve the pregnancy tissue or surgery to remove the ectopic pregnancy and repair any damage to the fallopian tube.
Pelvic Adhesions
Pelvic adhesions are bands of scar tissue that form between pelvic organs or between organs and the abdominal wall. These adhesions can develop following pelvic surgery, infections (such as pelvic inflammatory disease), or endometriosis.
Sharp or pulling pain in the pelvic area may occur as adhesions restrict movement of the affected organs, causing discomfort during physical activities or intercourse. In severe cases, pelvic adhesions can lead to bowel or bladder obstruction.
Treatment options vary and may include laparoscopic surgery to remove adhesions or manage symptoms.
Treatment options
Treatment for sharp pain in the vaginal area depends largely on the underlying cause identified through a thorough medical evaluation. Once the cause is determined, healthcare providers tailor treatment to address specific conditions effectively. For instance, infections such as pelvic inflammatory disease (PID) or urinary tract infections (UTIs) typically require antibiotics to eradicate bacterial pathogens.
Conditions like ovarian cysts or uterine fibroids may necessitate monitoring with imaging studies or surgical intervention if symptoms persist or worsen. Chronic conditions such as endometriosis or vulvodynia may benefit from a combination of pain management strategies, hormonal therapies, physical therapy, or surgical procedures to alleviate symptoms and improve quality of life.
Each treatment approach aims to alleviate pain, manage symptoms, and address any underlying factors contributing to the sharp pain in the vaginal area. Regular follow-up and collaboration with healthcare providers are essential to monitor progress and adjust treatment plans as needed.
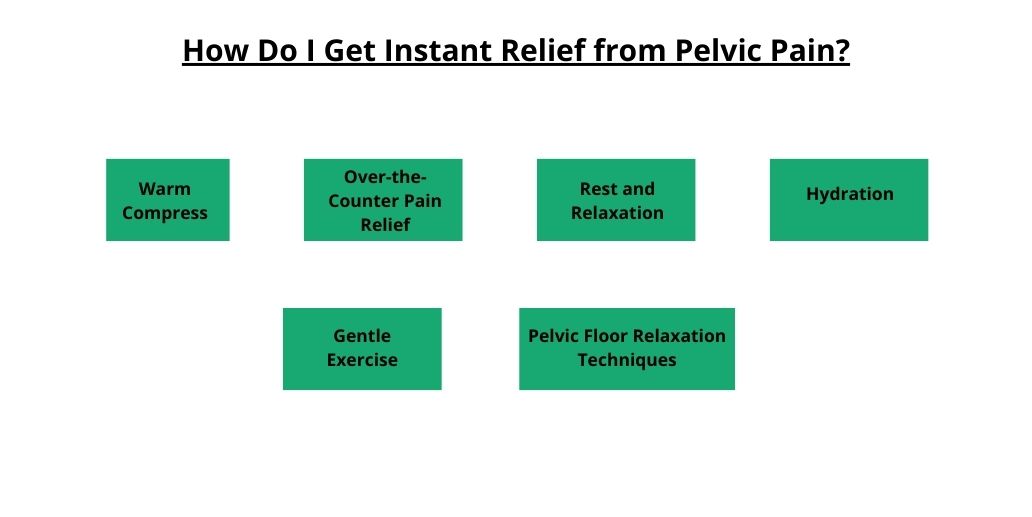
How Do I Get Instant Relief from Pelvic Pain?
Finding relief from sudden or persistent pelvic pain can be crucial for managing discomfort and improving daily functioning. While instant relief may not always be possible depending on the underlying cause, there are several strategies and home remedies that may help alleviate discomfort temporarily:
Warm Compress: Applying a warm compress or heating pad to the pelvic area can help relax muscles, increase blood flow, and reduce pain sensation.
Over-the-Counter Pain Relief: Non-prescription pain relievers such as ibuprofen (Advil, Motrin) or acetaminophen (Tylenol) can provide temporary relief from mild to moderate pelvic pain.
Rest and Relaxation: Taking time to rest in a comfortable position, such as lying down with pillows under the knees, can relieve pressure on the pelvic area and reduce pain intensity.
Hydration: Drinking plenty of water helps maintain bladder and bowel function, which can alleviate pelvic pain associated with urinary tract infections or constipation.
Gentle Exercise: Light stretching or gentle exercise, such as walking or yoga, can promote circulation and alleviate muscle tension in the pelvic area.
Pelvic Floor Relaxation Techniques: Practicing relaxation techniques such as deep breathing or pelvic floor exercises (Kegel exercises) can help relax tense muscles and reduce pelvic pain.
Closing Note
Addressing sharp shooting pain in the private area among females is crucial for their health and well-being. This type of pain can signal a range of conditions, from benign issues to more serious health concerns. Prompt medical evaluation and proper diagnosis are essential to determine the cause and initiate effective treatment.
Whether the pain is due to infections like PID or UTIs, gynecological conditions such as ovarian cysts or endometriosis, or other factors, timely intervention can alleviate discomfort and prevent complications.